Rheumatoid arthritis (RA) is a common, chronic polyarthritis which may be classified as a diffuse, multi-system, connective tissue disease. The hallmarks of RA are positive testing for immunoglobulin M (IgM) rheumatoid factor; bilateral, usually symmetrical joint disease; erosive changes noted radiographically; and persistent inflammatory synovitis.
 Incedence, Distribution, And Control Of Disease In Populations
Incedence, Distribution, And Control Of Disease In Populations
The prevalence of RA in the population is approximately 1%, and increases with increasing age. Women are affected about three times more frequently than men, although this gender difference is reversed in children. RA has a worldwide distribution. A genetic predisposition does seem to exist, as first-degree relatives of persons with seropositive erosive disease are five to six times more likely to develop severe RA. A strong association with the major histocompatibility complex gene product, HLA-DR4, and a preponderance of whites and Japanese with classic or definite RA have been demonstrated.
The Scientific Study Of The Nature Of Disease and Its Causes, Processes, Development, And Consequences.
Various theories have been advanced to explain RA, including infective agents, cellular hypersensitivity, genetic predisposition, and immune complex involvement. None has gained unequivocal acceptance. the exact role of rheumatoid factor is still uncertain.
A probable early event in the disease process is an antigen-antibody reaction at the synovial level with activation of complement. Acute pathological findings include micro-vascular injury; edema of subsynovial tissues; and synovial lining cell proliferation.
In established disease pathological examination of the synovium reveals edema, villous synovial rpojections, and hypertrophy and hyperplasia of the synovial lining cells (both A and B type cells). Vascular changes such as capillary obstruction, nuetrophil infiltration, areas of thrombosis, and perivascular hemorrhage are common. Mononuclear cells predominate in the synovial stroma. Mechanisms favoring and/or resulting in a chronic disease process are unknown. As inflammation contineus, pannus, an inflammatory synovial mass, is laid down. Pannus may ultimately invade bone and cartilage and lead to joint damage.
Clinical Features
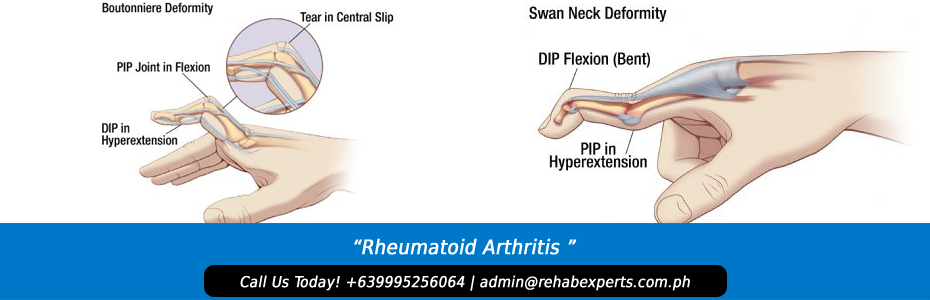
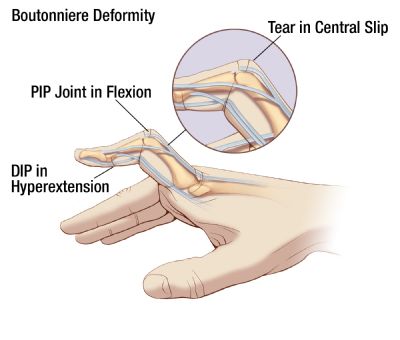
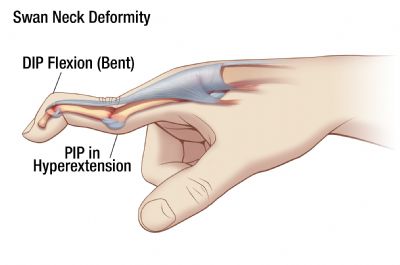
The onset of RA is usually gradual; however, 15 to 20% of patients experience it suddenly. Symptoms such as fatigue, anorexia, malaise, weight loss, weakness and generalized “aches and pains” usually herald the onset of RA. RA is iniatially polyarticular in approximately 75% of patients. The small joints of the hands and feet are most affected. Ultimately the hand involvement predominates, with PIP joints affected in 85% of patients, metacarpophalangeal (MCP) joints in 70%, and wrist in 80%. Other joints such as the knees, cervical spine, feet, and temporomandibular are commonly, though less frequently, affected.
Clinical features of involved joints include pain, swelling, limitation of movement, stiffness, and various signs of inflammation, such as erythema and synovitis. Morning stiffness, considered a result of synovial congestion, joint capsule thickening, and an increased volume of synovial fluid, is common.
The clinical course of RA is highly variable. Approximately 10% of patients have a mild, transient polyarthritis followed by a lasting remission; less than 10% have destructive polyarthritis. The remaining 80% exhibit a characteristic waxing and waning of symptoms. The degree of articular severity and the presence of extra-articular manifestations generally do not correlate; however, both of these are more likely to be severe in patients with high titers of rheumatoid factor.
Patients rarely die of RA. Death results typically from associated features such as vasculitis, cervical spine subluxation, complications of drug therapy, and infection. The course of the disease naturally varies with the individual patient, but certain aspects indicate a less favorable outcome. These include insidious onset (patients who perhaps present too late), youthful onset, being female and/or being Caucasian, seropositivity, rheumatoid nodules, and high titers of rheumatoid factor, C-reactive protein and/or haptoglobin.
The term “symmetrical,” used radiologically, refers to bilateral joint involvement, though not necessarily to the same degree. Bony ankylosis is rarely a feature.
Management
A management profile of rheumatoid arthritis can serve as a genetic model for physiatric care of the arthritides. Comprehensive management of the arthritis patient involves prescription of appropriate medications as well as utilization of a variety of resources familiar to physiatrist. Aspirin, in doses of 3 to 6 grams daily, is the accepted initial drug of choice. Begin at a dosage of 0.9 gram orally QID (4x/day) and increase gradually each 4 to 5 days as tolerated. Obtain serum salicylate levels (22-30mg/dl) periodically. A level producing tinnitus obviously needs to be reduced. Doses below 3 grams/day are usually only analgesic.
If aspirin is contraindicated, cannot be tolerated, or does not produce the desired therapeutic effect, a trial of non-steroidal anti-inflammatory agents (NSAIDs) is indicated. If these agents fail to suppress the disease process, a variety of such as gold, steroids, penicillamine, and antimalarials are available, in addition to a variety of experimental drugs and procedures. Consultation with a rheumatologist is recommended at this level of disease management.
Physical Rehabilitation
The physical rehabilitation team is familiar with the wide array of resources available for optimal treatment of arthritis patients.
The goals of arthritis rehabilitation are to:
- maintain or improve range of motion;
- prevent deformities;
- limit disability;
- protect susceptible joints;
- decrease pain and stiffness;
- use joints and muscles efficiently and safely;
- improve strength in selected muscles;
- improve endurance; and
- control weight and maintain appropriate nutrition.
Efficient arthritis rehabilitation is characterized by a motivated, well-informed patient, following a regimen prescribed and coordinated by a knowledgeable physician administered by a registered, well-trained therapist, and coordinated with other medical/surgical treatments. The regimen should include sufficient instructional treatments, an ongoing basic home program, and modification of the program as disease state changes. Poor rehabilitation outcome can result from the omission of these elements. Formal treatments that do not provide functional improvement or relief after several weeks should either be modified or discontinued. the patient and family should be aware that physical medicine and rehabilitaion (PM&R) treatments do not cure arthritis, substitute for adequate rest, replace prescribed medications, or usually result in rapid improvement.
Agents used for arthritis rehabilitaion include heat, cold, hydrotherapy, exercise, rest, mechanical agents, education, and/or other agents.
[tagline_box link=”http://www.rehabexperts.com.ph/contact-us” linktarget=”” button=”Contact us now!” title=”Physical Therapy Home Service” description=”Are you a person suffering from some physical disabilities? Do you intend to find a solution to your physical disabilities? Are you already tired masking the pain and intend to find a solution to your physical disabilities? Do you intend to address the root-cause of pain and find a lasting remedy to your physical disabilities? Are you looking for a good quality physical therapy home service?”][/tagline_box]