Bell’s Palsy is the paralysis or severe weakness of the nerve that controls the facial muscles on the side of the face – the facial nerve or seventh cranial nerve. Patients typically find they suddenly cannot control their facial muscles, usually on one side.
A person might have Bell’s Palsy first thing in the morning – they wake up and find that one side of the face does not move. If an eyelid is affected, blinking might be difficult.
Bell’s Palsy usually starts suddenly.
Most people who suddenly experience symptoms think they are having a stroke. However, if the weakness or paralysis only affects the face it is more likely to be Bell’s palsy.
Neurology / Neuroscience News Section
Bell’s palsy is named after Charles Bell, a Scottish anatomist who first described it in 1821, and published his findings in a Royal Society paper entitled “On the Nerves: Giving an Account of some Experiments on Their Structure and Functions, Which Lead to a New Arrangement of the System”.
According to Medilexicon’s medical dictionary, Bell’s palsy is “paresis or paralysis, usually unilateral, of the facial muscles, caused by dysfunction of the seventh cranial nerve; probably due to a viral infection; usually demyelinating in type.”
What are the symptoms of Bell’s palsy?
The facial nerves control blinking, opening and closing of the eyes, smiling, salivation, lacrimation (production of tears), and frowning. They also supply the stapes muscles with nerves. The stapes is a bone in the ear which is involved in our ability to hear. When the facial muscle malfunctions, the following symptoms may emerge – symptoms of Bell’s palsy:
- Sudden paralysis/weakness in one side of the face.
- It may be difficult or impossible to close one of the eyelids.
- Irritation in the eye because it does not blink and becomes too dry. Changes in the amount of tears the eye produces.
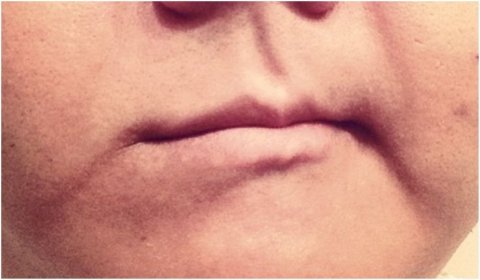
- Parts of the face may droop, such as one side of the mouth.
- Drooling from one side of the mouth. The amount of saliva produced changes.
- Difficulty with facial expressions.
- Sense of taste may become altered.
- An affected ear may lead to sensitivity to sound (hyperacusis). Sounds seem louder.
- Pain in front or behind the ear on the affected side.
- Headache.
What causes Bell’s palsy?
The facial nerve controls most of the muscles in the face and parts of the ear. The facial nerve goes through a narrow gap of bone from the brain to the face. This nerve becomes inflamed.
We are not completely certain what the cause of Bell’s palsy is.
A virus – experts believe it is most likely caused by a virus, usually the herpes virus, which inflames the nerve. The herpes virus is the one that also causes cold sores and genital herpes. Other viruses have also been linked to Bell’s palsy, including the chickenpox and shingles viruses, which are both related to the herpes virus. The virus that causes mononucleosis (Epstein-Barr) as well as the cytomegalovirus have also been linked to Bell’s palsy. Lyme disease in areas where it is endemic may be a principal cause of Bell’s palsy type symptoms caused by bacteria.
If the nerve is inflamed it will press against the cheekbone or may pinch in the tight corridor (narrow gap of bone) – this can result in damage to the protective covering of the nerve.
If the protective covering of the nerve becomes damaged, the signals which are being sent from the brain to the muscles in the face may not be transmitted properly, leading to weakened or paralyzed facial muscles – Bell’s palsy.
How is Bell’s palsy diagnosed?
Diagnosing by a process of elimination (diagnosis of exclusion)
The doctor will look for evidence of other conditions which may be causing the facial paralysis, such as a tumor, Lyme disease, or stroke. This will involve checking the patients head, neck and ears. He/she will also check the facial muscles carefully and determine whether any other nerves are affected apart from the facial nerve.
If there is a change in facial structure it could be evidence of a tumor. A characteristic rash may be evidence of tick bites in Lyme disease.
If all other causes can be excluded, the doctor will diagnose Bell’s palsy. If the doctor is still unsure, the patient may be referred to an ENT (ear, nose and throat) specialist – an otolaryngologist. The specialist will examine the patient and may also order the following tests:
- Electromyography (EMG) – electrodes are placed on the patient’s face. A machine measures the electrical activity of the nerves – and the electrical activity of a muscles in response to stimulation. This test can determine the extent of nerve damage, as well as its location.
- MRI, CT scans or X-rays – these are good at determining whether other underlying conditions are causing the symptoms, such as a bacterial infection, skull fracture, or a tumor.
What are the complications of Bell’s palsy?
It is important to stress that the vast majority of patients with Bell’s palsy make a full recovery. However, if damage to the facial nerve is severe some complications are possible, including:
- Misdirected re-growth of nerve fibers – nerve fibers re-grow in an irregular way. This can result in involuntary contractions of some muscles. A patient may involuntarily close one eye when trying to smile. The problem might be the other way round – when the person closes one eye, the side of the mouth lifts involuntarily.
- Ageusia – chronic (long-lasting) loss of taste.
- Gustatolacrimal reflex – also known as crocodile tear syndrome. While the patient is eating his/her eye will shed tears. It is estimated to occur in about 6% of patients during recovery, and eventually goes away. In some rare cases the problem can be longer lasting.
- Corneal ulceration – when eyelids cannot completely shut, the protective and lubricating tear film of the eye may become ineffective. This can result in corneal drying. The risk or corneal drying is even higher if Bell’s palsy has also caused a reduction in tear production. Corneal ulceration can result in infection of the cornea, which can lead to severe loss of vision.
How Can a Physical Therapist Help?
In the first couple of days to a week after symptoms start, your physical therapist will evaluate your condition, including:
- Review your medical history, and discuss any previous surgery or health conditions
- Review when your current symptoms started and what makes them worse or better
- Conduct a physical examination, focusing on identifying the patterns of weakness that are caused by Bell palsy:
- Facial movements of the eyebrow
- Eye closure
- Ability to use the cheek in smiling
- Ability to use the lips in a pucker
- Ability to suck the cheeks between the teeth
- Raising the upper lip
- Raising or lowering the lower lip
Your physical therapist will immediately:
- Educate you about how to protect your face and your eye
- Show you how to manage your daily life functions while you have facial paralysis
- Explain the expected path to recovery, so that you will know the signs and symptoms of recovery
- Evaluate your progress, and determine whether you need to be referred to a specialist if progress is not being made
The first priority is to protect your eye. The inability to completely and quickly close your eye makes the eye vulnerable to injury from dryness and debris. Debris can scratch the cornea—the transparent front part of the eye that covers the iris, pupil, and front chamber of the eye—and could permanently harm your vision. Your physical therapist will immediately show you how to protect your eye, such as:
- Using self-made and commercial patches
- Setting a regular schedule for refreshing eye fluids
- Carefully closing the eye with your fingers
If you have partial facial movement, your therapist will teach you a few general facial exercises to do at home. These exercises will help you learn to move the weak side of your face and help you use both sides of your face together. One of the exercises is a gentle blowing action through your lips.
During Recovery
Your physical therapist will help you regain the healthy pattern of movements that you need for facial expressions and function. Recovery can be challenging because:
- Normally, the ability to make facial expressions and many facial movements is “automatic”;—that is, you’re born with this ability and never had to think about it before
- Unlike other muscles in your body, the facial muscles do not have sensors that tell your brain all of the necessary “details” about how to move
Your physical therapist will be your coach throughout this challenging time, guiding you through special exercises that are designed to help you relearn facial movements based on your particular movement problems. Your exercises may change over the course of recovery:
“Initiation” exercises. In the early stages, when you might have difficulty producing any facial movement at all, your therapist will teach you exercises that cause (“initiate”) facial movement. Your therapist will show you how to position your face to make it easier to move (called “assisted range of motion”) or how to “trigger” the facial muscles to do what you want them to do.
“Facilitation” exercises. Once you’re able to initiate movement of the facial muscles, your therapist will design exercises to increase the activity of the muscles, strengthen the muscles, and improve your ability to use the muscles for longer periods of time (“facilitate” muscle activity).
Movement control exercises. Your therapist will design exercises to:
- Improve the coordination of your facial muscles
- Refine your facial movements for specific functions, such as speaking or closing your eye
- Refine movements for facial expressions, such as smiling
- Correct abnormal patterns of facial movement that can occur during recovery
To work on coordinating your facial muscles, you’ll need to have a sufficient level of activation of facial muscles first. Your therapist will determine when you’re ready.
Relaxation.During recovery, you might have facial spasms or twitches. Your physical therapist will design exercises to reduce this unwanted muscle activity. The therapist will teach you how to recognize when you are activating the facial muscle and when the muscle is at rest. By learning to contract the facial muscle forcefully and then stop, you will be able to relax your facial muscles at will and decrease twitches and spasms.
After Recovery
Some people might have greater difficulty moving their face after a period of improvement in facial movement, which can make them worry that the facial paralysis is returning. However, actual recurrence of facial paralysis of the Bell Palsy type is uncommon.
New difficulty in moving the face is more likely the result of increasing the strength of the facial muscles without improving the ability to coordinate and control the movement. To keep this from happening, your physical therapist will show you what facial movements you should avoid during recovery. For instance, the following might lead to abnormal patterns of facial muscle use:
- Trying to make the biggest facial movement or muscle contraction that you can, such as smiling as much as you can
- Chewing gum with great force
- Blowing up a balloon with all of your effort to work the facial muscles
Your therapist will coach you to use your face as naturally as possible, without trying to restrict facial expressions because they look “different.”
Reference:
Medical News Today http://www.medicalnewstoday.com/articles/158863.php
Move Forward http://www.moveforwardpt.com/symptomsconditionsdetail.aspx?cid=96135873-1b28-48bc-8be7-7d05c334daf1
[tagline_box link=”http://www.rehabexperts.com.ph/contact-us” linktarget=”” button=”Contact us now!” title=”Physical Therapy Home Service” description=”Are you a person suffering from some physical disabilities? Do you intend to find a solution to your physical disabilities? Are you already tired masking the pain and intend to find a solution to your physical disabilities? Do you intend to address the root-cause of pain and find a lasting remedy to your physical disabilities? Are you looking for a good quality physical therapy home service?”][/tagline_box]