The post Patient With Hemiplegic Condition appeared first on Rehab Experts.
]]>The word ‘plegia‘ means weakness so severe that it is nearly complete. ‘Hemi‘ implies one side of the body. Hence, ‘hemiplegia‘ means complete paralysis of one half of the body, including one arm and leg. Any disease or injury in the motor centers of the brain can cause hemiplegia.
Hemiplegia is a more severe form of ‘hemiparesis‘ wherein one half of the body is only weakened. It is also very different from the conditions of paraplegia & quadriplegia, which are commonly confused with hemiplegia. Paraplegia is paralysis in both legs, below the waist. Quadriplegia is paralysis below the neck and is also usually the result of a spinal cord injury.
Causes of Hemiplegia
Many conditions give rise to hemiplegia. Generally, an injury to the right side of the brain will cause a left-sided hemiplegia while an injury to the left side of the brain will cause a right-sided hemiplegia.
- Stroke: is the commonest cause of hemiplegia. Insufficient blood supply to the brain leads to loss of brain functions. The stroke may be caused by:
- A clot formed within the blood vessel blocking the blood supply’-> a thrombus
- A thrombus breaks away from its site of origin and forms a block elsewhere in the circulation. -> an emboli
- A bleed from a blood vessel supplying the brain -> a hemorrhage
- Head injury
- Diabetes
- Brain tumor
- Infections -> meningitis, encephalitis
- Migraine syndrome -> recurrent headaches of severe intensity occasionally accompanied by sensations of numbness and tingling in one half of the body.
- Inflammation of the blood vessels -> vasculitis
- Diseases affecting the nerves -> like Multiple Sclerosis; acute necrotizing myelitis.
- Conditions presenting from birth -> cerebral palsy. Lack of blood supply damages nerve cells in the brain. Birth trauma, difficult labor, perinatal strokes in infants within 3 days of birth can all cause cerebral palsy.
- Hereditary diseases -> leukodystrophies. This is a rare disorder affecting the myelin sheath which covers and protects nerve cells in the brain. The condition usually appears in infancy or childhood.
Symptoms of hemiplegia
Injury or insults to the brain cells that control movements in one half of the body cause hemiplegia. Hence, symptoms largely depend upon the part of the brain affected. The same can be said about the severity of individual symptoms.
- Difficulty in walking.
- Problems in balance, losses balance when trying to walk
- Difficulty in swallowing
- Trouble with vision. Blurred vision or weakness of the eyes.
- Speech becomes difficult.
- Numbness, tingling or loss of sensations on one half of the body.
- Loss of control over bladder and bowel movements leading to an inability to hold on to stool or urine.
- Unable to perform tasks like holding objects, tying laces, dressing oneself, buttoning etc.
- Feeling depressed
- Heightened emotional sensitivity with inability to handle stressful situations.
- Memory seems poor. Unable to recall recent or past events concerning people, places and activities.
The presentation will also depend on which side of the brain is damaged.
- Right hemiplegia is caused by damages n the left hemisphere while with left hemiplegia it is vice versa.
- Right hemiplegia most often shows -> loss of sensations on left side. There will be difficulty in understanding the spoken or written word -> condition called aphasia.
- Left hemiplegia often presents itself after right cerebral hemisphere damage. It usually presents with
- Loss of control over purposeful movements.
- Unable to use objects correctly.
- Unable to draw, comb hair or cook.
Conditions like Alternating Hemiplegia have recurring episodes of hemiplegia. But, attacks are generally preceded by warning symptoms like –
- Yawning
- Fatigue
- Appearing very exhausted
Pure hemiplegia has to be differentiated with Alternating Hemiplegia that affects children. Though relatively rare, this condition has recurring episodes of weakness in one half of the body alternating with periods when there are no weaknesses. During an attack, the child may suffer from the many symptoms of a stroke. They may develop long term sequelae like movement disorders and behavior problems.
Diagnosis
Doctors may want a few procedures done to find the cause of hemiplegia. Some required tests are:
- Complete blood count.
- Blood biochemistry test.
- Cranial CT -> a highly detailed, non-invasive, imaging procedure that combines x-rays with computer technology and allows the study of the brain from many angles.
- Cranial MRI -> a non-invasive, highly sensitive procedure that uses electromagnetic properties of tissues providing detailed studies of their structures.
- An EEG (electroencephalogram) -> can measure the nerve activity within the brain.
Rehabilitation
Individuals who suffer from hemiplegia may require various rehabilitation services, including physical therapy, occupational therapy, speech therapy, and orthotic management. Rehabilitation services should occur at a frequency of 2 to 3 times a week.
Occupational therapy focuses on regaining the ability to perform activities of daily living. Individuals learn to perform tasks while sitting down on a kitchen stool. By instructing individuals in tasks such as these, occupational therapists also engage in balance retraining. Individuals also learn dressing and bathing techniques. Occupational therapists may order equipment to assist individuals.
Occupational therapists also promote the return of upper extremity and hand function through a variety of activities. Often the upper arm separates (subluxes) from the shoulder girdle because of a loss of muscle tone. Occupational therapy may use neuromuscular electrical stimulation (NMES), in which electrodes provide external stimulation to the muscles to counteract this symptom. More frequently, individuals wear a hemi-sling that helps support the arm to prevent subluxation. Occupational therapists may stretch the upper extremities and teach self-stretching techniques so that the arm can regain maximum potential. Individuals also learn strengthening exercises and practice tasks that require the affected hand to bear weight, thus sending nerve impulses to the brain so that damaged neural paths can begin to heal. Individuals engage in tasks that require both hands, such as holding a cup with the hemiplegic hand while pouring a drink using the good hand. As function returns, individuals may engage in fine motor tasks such as handwriting.
Occupational therapists also are instrumental in helping an individual perform activities of daily living, such as housecleaning, gardening, and practicing arts and crafts. They also help individuals learn how to adapt to driving and provide on-road training, which may be an important consideration in returning to work.
Physical therapy focuses on stretching and strengthening the hemiplegic side. Therapists may passively stretch the affected side. Individuals and their family members learn to perform a stretching and strengthening program for the legs. Physical therapy also focuses on transfer training. The therapist teaches the individual to bear weight evenly when sitting and standing so that the individual is aware of the hemiplegic side. Individuals also learn mobility techniques such as walking and climbing stairs while using a pyramid cane or 4-pronged cane. For those individuals who cannot walk, the physical therapist may order a special wheelchair, called a hemi-chair, which can be propelled using only the good arm because a special axle connects the wheels.
Orthotic management may also be required for individuals to regain function. Occupational therapists may make an individual a night splint, which positions the thumb and fingers so that the hand forms the letter “C.” This position places the hand in a functional position, allowing for full use of the hand if strength returns. An orthotist, who custom-fits braces and splints, may make an individual a leg splint to promote better control of the ankle and knee during ambulation.
Speech therapy may be required to strengthen the muscles of the face for improved speech and swallowing. Individuals learn to move the facial muscles in a balanced manner, both by manual assistance and visual cueing through the use of a mirror. Individuals perform tongue exercises to allow for better speech and eating. Activities such as sustained vocal expressions help individuals learn to speak with greater clarity. Individuals begin eating semi-moist, pureed food, which is easier to swallow, and progress to eating food rich in taste, smell, and texture to assist in the swallowing reflex. Individuals also learn to achieve sucking control and saliva production.
Reference
Life Force http://www.askdrshah.com/app/hemiplegia.asp
MD Guidelines http://www.mdguidelines.com/hemiplegia
The post Patient With Hemiplegic Condition appeared first on Rehab Experts.
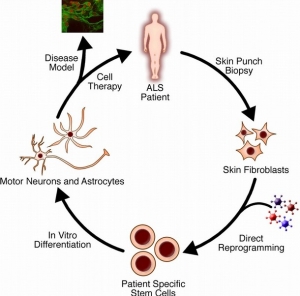
]]>The post Amyotrophic Lateral Sclerosis (ALS) appeared first on Rehab Experts.
]]>Amyotrophic lateral sclerosis (ALS), sometimes called Lou Gehrig’s Disease, is a progressive brain disease that attacks the nerve cells (neurons) that control voluntary muscles. This disease belongs to a group of motor neuron disorders (e.g., muscular dystrophy, multiple sclerosis, Parkinson’s disease) that lead to the gradual degeneration and death of motor neurons, the nerve cells located in the brain, brainstem, and spinal cord. These motor neurons serve as connections from the nervous system to the muscles in the body.
Imagine wanting to brush your teeth. The motor neurons in the brain (upper motor neurons) have to send a message to the motor neurons in the spinal cord (lower motor neurons). The lower motor neurons then send the message to the muscles that are needed to brush your teeth (arms, mouth, etc.). ALS causes both the upper and lower motor neurons to degenerate or die. Both the brain and spinal cord lose the ability to initiate and send messages to the muscles in the body. The muscles, which are unable to function, gradually atrophy (waste away) and fasciculate (twitch).
ALS does not impair a person’s mind. It affects only the motor neurons. Personality, intelligence, memory, and self-awareness remain the same. The senses of sight, smell, touch, hearing, and taste remain intact as well.
What are some signs or symptoms of ALS?
ALS first affects an individual’s ability to speak loudly and clearly. Eventually, it completely prevents speaking and vocalizing. Some of the earliest speech-related symptoms of ALS may include:
- nasal speech quality (talking out of your nose)
- difficulty pronouncing words due to weak, tight, or stiff speech muscles (dysathria)
- difficulty with lengthy sentences or conversation
As muscles for breathing weaken, it becomes more difficult for patients to speak loud enough to be understood. Eventually extensive muscle atrophy eliminates one’s ability to vocalize and speak altogether.
Patients may also experience difficulty chewing and swallowing. Initially only some food consistencies are affected, but over time it becomes difficult for the patient to swallow even pureed foods and saliva. People with ALS get tired easily and they may not have the energy to eat an entire meal. All of these factors make it difficult to maintain adequate nutrition and weight. Eventually doctors may decide that it is best to insert a feeding tube into the person’s stomach to make sure they receive enough nutrition.
In some cases, initial symptoms affect only one leg or arm. Patients may have awkwardness and stumbling when walking or running. They may have difficulty lifting objects or with tasks that require manual dexterity (e.g., buttoning a shirt, tying a shoe, turning a key). Eventually the individual will not be able to stand or walk, get in and out of bed without help, or use hands and arms to perform activities of daily living, such as washing and dressing.
How is ALS diagnosed?
There is no specific laboratory test for ALS, making it hard to diagnose. The diagnosis is made using clinical findings in conjunction with results of electrodiagnostic studies and the absence of evidence of other disorders. According to the diagnostic guidelines of the World Federation of Neurology, there must be lower motor neuron degeneration detected by clinical electrophysiological or neuropathologic examination, signs of upper motor neuron degeneration by clinical examination, and progressive spread of signs within a region of the body or to other regions.
Causes of ALS
The cause of ALS is unknown, though some cases where there’s a family history of the disease are associated with mutations in the gene for an enzyme called SOD1. It’s not clear how the mutations cause motor neuron degeneration, but studies suggest the SOD1 protein can become toxic.
Scientists have identified more than a dozen other genetic mutations that may be linked to ALS. These mutations cause changes in the processing of RNA molecules (which may regulate genes), defects in the recycling of proteins, defects in motor neuron shape and structure, or susceptibility to environmental toxins.
Other research suggests ALS may share similarities to frontotemporal dementia (FTD), a degenerative disease of the brain’s frontal lobe. A defect in the C9orf72 gene is found in a substantial number of ALS patients as well as some FTD patients.
Respiratory complications
All deaths directly caused by ALS result from respiratory complications. This occurs primarily from the patient’s inability to ventilate as respiratory muscle weakness progresses. In patients with bulbar weakness, aspiration of secretions or food may occur and precipitate pneumonia, resulting in further respiratory compromise; therefore, aggressive respiratory management is necessary in the comprehensive care of patients with ALS.
Routinely measure vital capacity in the sitting and recumbent positions. Most often, the recumbent measurement declines prior to the sitting measurement. Gravity assists in lowering the diaphragm as the patient’s angle of inclination is increased. As respiratory weakness progresses, patients have increasing difficulty with diaphragmatic movement when supine because of the elimination of this effect from gravity. This results in alveolar hypoventilation and ultimate oxyhemoglobin desaturation.
Difficulty sleeping may be the first symptom of hypoventilation. Patients should be questioned routinely regarding sleep habits, and if a sleep disturbance develops, measure vital capacities sitting and supine. In addition, perform overnight oxygen saturation monitoring to assess for nocturnal hypoxemia and the need for nocturnal noninvasive intermittent positive pressure ventilation (IPPV).
Treatment for ALS
Currently, ALS does not have a cure, but treatments exist to relieve symptoms and improve patients’ quality of life.
The first drug for treating the disease, Riluzole, was approved by the Food and Drug Administration (FDA) in 1995. Riluzole is thought to decrease damage to the motor neurons by minimizing the release of the chemical signal glutamate. In clinical trials, the drug prolonged the survival of ALS patients’ (particularly ones who had difficulty swallowing) by several months. It can extend also the time before a patient must go on a ventilator.
Doctors can prescribe medications for reducing fatigue, muscle cramps, muscle spasticity, and excessive saliva or phlegm, as well as pain, depression, sleeping problems or constipation.
Speech therapists and nutritionists can help ALS patients who have trouble speaking or swallowing. As the disease advances, patients can learn to answer yes-or-no questions with their eyes or using computer-based systems.
Physical Therapy and Exercise
Physical exercise can help maintain or improve strength in the muscles not affected byALS, and maintain flexibility in muscles which are affected. It can help prevent stiffness in the joints. Physical therapy may also help people with breathing difficulties to clear their chests and maintain lung capacity. However, people living with ALS can tire very easily and find they need to conserve energy, so very strenuous exercise is not normally recommended.
Several people had found physical therapy and gentle exercise helpful, including hydrotherapy or swimming. A few had continued going to the gym and had adapted their exercise routine as their symptoms changed. Special equipment — such as ramps, braces, walkers and wheelchairs — can give patients mobility without exhausting them.
Physical therapists should instruct proper stretching and daily range-of-motion (ROM) exercises to the patient with amyotrophic lateral sclerosis (ALS) and his/her caregivers. Therapists should try to anticipate the patient’s future needs and introduce assistive devices in a timely manner. Lightweight ankle-foot orthoses can be provided to minimize foot drop and stabilize weak quadriceps muscles to prevent falls.
The physical therapist should also emphasize energy conservation and teach patients and caregivers methods for performing safe, efficient transfers. Therapists also can provide instruction for strengthening exercise programs, but exercises should be performed at submaximal levels in muscles without marked weakness and should be prescribed only for patients with slowly progressive disease.
In one study, individualized, moderate-intensity, endurance-type exercises for the trunk and limbs performed 15 minutes twice daily was shown to significantly reduce spasticity as measured by the Ashworth scale. The effects of exercise in people with ALS are not well understood. A recent Cochrane review concluded that studies were too small to determine to what extent strengthening exercises for people with ALS are beneficial or whether exercise is harmful. There is a complete lack of randomized or quasi-randomized clinical trials examining aerobic exercise in this population.
When making wheelchair recommendations, the therapist should try to anticipate the patient’s future needs. Wheelchairs should be introduced while the patient is still ambulatory in order to enhance energy conservation. Initially, a lightweight wheelchair should be rented, with plans to purchase a heavier, more expensive chair when the patient is no longer able to ambulate. Recommend modifications to the patient’s wheelchair in a timely manner and in accordance with the patient’s tolerance for gadgets.
Occupational Therapy
Occupational therapists should focus on teaching energy conservation techniques to the patient with amyotrophic lateral sclerosis (ALS) and his/her caregivers. Adaptive equipment should be introduced early and in synchronization with the patient’s progressing needs.
Upper extremity bracing can be used in cases where weakness may alter joint biomechanics. Patients with poor grasp can be provided with a universal cuff, and patients with hand weakness can be braced in 20-25° of extension to improve grip strength. For patients with proximal upper extremity weakness, a balanced forearm orthosis (ie, deltoid aid) may be beneficial to enhance upper extremity movement by eliminating the effects of gravity. When shoulder girdle weakness progresses to advanced stages, slings can be used to decrease pain by limiting traction on the associated ligaments, nerves, and vessels.
For patients with severe limb involvement, introduce environmental control units (ECUs) that utilize oral-motor movements. In patients with severe bulbar involvement, extraocular movements are usually preserved so ECUs incorporating eye gaze technology can be used.
Reference:
American Speech-Language Hearing Association http://www.asha.org/public/speech/disorders/als/
Live Science http://www.livescience.com/39583-als-lou-gehrigs-disease.html
Medscape http://emedicine.medscape.com/article/306543-overview#aw2aab6b4
Health Talk Online http://healthtalkonline.org/peoples-experiences/nerves-brain/motor-neurone-disease/physical-therapy-and-exercise
The post Amyotrophic Lateral Sclerosis (ALS) appeared first on Rehab Experts.
]]>The post Peripheral Nerve Injury appeared first on Rehab Experts.
]]>Peripheral nerves are vulnerable to injury by many means. Diabetes and traumatic or repetitive strain injury are among the most common causes of peripheral nerve damage. Infections, autoimmune disorders, exposure to toxins, nutritional deficiencies, and hereditary conditions are among myriad other causes of neuropathy.
Peripheral neuropathies can affect motor neurons (which control intentional muscle movement), sensory neurons (which provide feedback to the brain from the muscles), and autonomic neurons (which control the muscles required for breathing, swallowing and other autonomic functions). Motor-nerve damage can lead to many mobility-limiting problems with the muscles, such as painful cramping, involuntary twitching, weakness, wasting, and complete or partial paralysis. Damage to sensory neurons can also affect mobility, due to sensations of numbness or pain and the loss of balance and sense of position. Such damage makes it difficult to coordinate the movements required to walk, get dressed, and perform other activities of daily living.
Some forms of peripheral nerve damaged can be managed with medication and/or physical therapy; others cannot. Approaches to treatment and research vary widely depending on the cause and type of damage. Mobility Project researchers are working on a novel strategy to restore hand movement in people with certain peripheral nerve injuries.
Clinical manifestations
The various clinical presentations of patients with peripheral nerve injuries are obviously dependent on the particular nerve or nerves that have been injured as well as the severity and level of the lesion. It is the case with the majority of traumatic peripheral nerve injuries that pain and loss of sensory and motor function are noted either immediately or within days of the inciting traumatic event.
Brachial plexus injuries. The clinical manifestations of brachial plexus injuries are particularly dependent on the specific elements of the plexus that have been injured. The plexus originates from the roots of C5 through T1. For the most part, the C5 root generally gives rise to deltoid function, the C6 root to biceps function, the C7 root to triceps function, the C8 root to the deep flexors of the hand and forearm, and the T1 root to the intrinsic muscle function of the hand. Using these motor functions as a guideline, along with the appropriate sensory distributions, the extent of injury can often be determined by clinical examination.
Median nerve injuries. The most significant and debilitating clinical manifestation of a median nerve injury is loss of pinch and grip strength secondary to denervation of the flexor pollicis longus muscle and the intrinsic muscles of the thenar eminence. A median nerve injury occurring high in its course through the arm will also decrease pronation strength, result in atrophy of forearm muscle mass, and cause sensation deficit of both the volar and palmar aspects of the lateral 3.5 digits.
Radial nerve injuries. The radial nerve originates in the distal axilla and is susceptible at that site to compression injuries, which produce “Saturday night palsy.” The hallmark of such a proximal radial nerve injury is the patient’s inability to extend the forearm secondary to loss of triceps innervation. The majority of radial nerve injuries occur at the midhumeral level secondary to fracture and present with sparing of triceps muscle function in the face of more distal radial distribution loss such as a wrist drop and inability to extend the fingers and thumb. Typically, the sensory deficits involved with radial nerve injury are minimal, involving only the dorsum of the hand and the anatomical snuffbox region.
Ulnar nerve injuries. The ulnar nerve receives its entire contribution from the medial cord of the brachial plexus. In an injury producing a total ulnar palsy, a patient will present with a classic hand posture in which there is partial flexion or “clawing” of the little finger and, to a lesser extent, the ring finger. In the case of a compression syndrome, sensory symptoms in the form of paresthesias and numbness in the little and ring fingers may be the patient’s first complaint. With time, patients will experience atrophy of the intrinsic muscles of the hand, producing a characteristic appearance and significant hand weakness.
Spinal accessory nerve injuries. In 1993, Donner and Kline found the 2 most common complaints of 83 patients with an extracranial spinal accessory nerve injury to be the inability to raise the arm above the horizontal plane and a “dragging pain” in the shoulder. The inability to raise the arm was secondary to a degree of trapezius weakness (particularly the upper trapezius) seen in all patients, whereas the dragging pain was thought to be due to downward tension on the shoulder joint secondary to chronic sagging of the shoulder. Also, on physical exam, scapular winging is a frequent finding distinguishable from the winging of serratus anterior palsy by its disappearance when the patient’s arm is raised forward, fully extended, and pushed against resistance.
Sciatic nerve injuries. Injury to the sciatic nerve at the proximal buttock level or more distally at the midthigh level can produce various symptoms depending on the amount of functional loss in the peroneal and tibial divisions of the nerve. The peroneal division lies posteriorly within the sciatic nerve making it prone to injury from injections or hip fractures. Patients will present with a foot drop secondary to loss of dorsiflexion and eversion of the foot as well as an inability to extend the toes. Injury to the tibial division of the sciatic produces loss of plantar flexion and inversion of the foot as well as loss of toe flexion. Patients with primarily tibial division injury complain mostly of a burning, hyperesthetic sole of the foot.
Femoral nerve injuries. The femoral nerve is the largest branch of the lumbar plexus, arising from the anterior divisions of L2, L3, and L4 spinal nerves. Injury to this nerve within the pelvis will produce a loss of hip flexion due to denervation of the iliopsoas muscle and a loss of knee extension secondary to denervation of the quadriceps muscles. Patients will find it difficult, if not impossible, to climb stairs with this injury. Injury to the femoral nerve at the level of the pelvis will produce a variable loss of hip flexion and variable sensory loss in the anteromedial thigh; however, absence of quadriceps function with loss of the patellar reflex will be uniform. Thigh-level injury of the femoral nerve within the region of the femoral triangle will also produce a complete loss of quadriceps function.
Peripheral Nerve Injury Rehabilitation
A physical medicine and rehabilitation (PM&R) physician, or physiatrist, often follows patients with peripheral nerve injuries as they go through the phases of healing, whether or not they require surgery. These specialists treat pain, if present, and help to minimize the functional deficits that can develop as a result of a peripheral nerve injury.
Pain is treated by a combination of means, including medication. The most effective medications interfere with pain nerve transmission, and are helpful in decreasing this purposeless output of injured nerves as they heal. Other pain treatments include injections of anesthetics, steroids, or other agents, and new technological devices that emit low-frequency signals masking pain nerve signals. Most types of pain can be greatly minimized by a combination of these means.
Preserving function after a peripheral nerve injury follows a careful examination which details the present capability of an affected area, as well as any vulnerable areas as a result of weakness or disuse. Range of motion of a joint within an affected area can be permanently lost if it is not maintained—even if nerve function is subsequently regained. Lack of joint protection can result in future traumatic arthritis, and thus pain. Modern technology has a furnished a number of assistive devices that can provide temporary independence, while safely protecting joints and zones of nerve healing. In addition, other well functioning areas can be helped to compensate for affected areas.
At Rehab Experts our physical therapists are specialized in the evaluation and treatment of nerve conditions. We develop individual treatment plans that are highly effective and we work with your physician for optimal results.
Reference:
Atlantic Mobility Action Project http://www.amap.ca/index.php?option=com_content&view=article&id=75&Itemid=72
Neurology Medlink http://www.medlink.com/medlinkcontent.asp
Columbia University Medical Center http://www.columbianeurosurgery.org/specialties/peripheral-nerve/treatment/peripheral-nerve-injury-rehabilitation/
The post Peripheral Nerve Injury appeared first on Rehab Experts.
]]>The post What Is Bell’s Palsy? What Causes Bell’s Palsy? appeared first on Rehab Experts.
]]>A person might have Bell’s Palsy first thing in the morning – they wake up and find that one side of the face does not move. If an eyelid is affected, blinking might be difficult.
Bell’s Palsy usually starts suddenly.
Most people who suddenly experience symptoms think they are having a stroke. However, if the weakness or paralysis only affects the face it is more likely to be Bell’s palsy.
Neurology / Neuroscience News Section
Bell’s palsy is named after Charles Bell, a Scottish anatomist who first described it in 1821, and published his findings in a Royal Society paper entitled “On the Nerves: Giving an Account of some Experiments on Their Structure and Functions, Which Lead to a New Arrangement of the System”.
According to Medilexicon’s medical dictionary, Bell’s palsy is “paresis or paralysis, usually unilateral, of the facial muscles, caused by dysfunction of the seventh cranial nerve; probably due to a viral infection; usually demyelinating in type.”
What are the symptoms of Bell’s palsy?
The facial nerves control blinking, opening and closing of the eyes, smiling, salivation, lacrimation (production of tears), and frowning. They also supply the stapes muscles with nerves. The stapes is a bone in the ear which is involved in our ability to hear. When the facial muscle malfunctions, the following symptoms may emerge – symptoms of Bell’s palsy:
- Sudden paralysis/weakness in one side of the face.
- It may be difficult or impossible to close one of the eyelids.
- Irritation in the eye because it does not blink and becomes too dry. Changes in the amount of tears the eye produces.
- Parts of the face may droop, such as one side of the mouth.
- Drooling from one side of the mouth. The amount of saliva produced changes.
- Difficulty with facial expressions.
- Sense of taste may become altered.
- An affected ear may lead to sensitivity to sound (hyperacusis). Sounds seem louder.
- Pain in front or behind the ear on the affected side.
- Headache.
What causes Bell’s palsy?
The facial nerve controls most of the muscles in the face and parts of the ear. The facial nerve goes through a narrow gap of bone from the brain to the face. This nerve becomes inflamed.
We are not completely certain what the cause of Bell’s palsy is.
A virus – experts believe it is most likely caused by a virus, usually the herpes virus, which inflames the nerve. The herpes virus is the one that also causes cold sores and genital herpes. Other viruses have also been linked to Bell’s palsy, including the chickenpox and shingles viruses, which are both related to the herpes virus. The virus that causes mononucleosis (Epstein-Barr) as well as the cytomegalovirus have also been linked to Bell’s palsy. Lyme disease in areas where it is endemic may be a principal cause of Bell’s palsy type symptoms caused by bacteria.
If the nerve is inflamed it will press against the cheekbone or may pinch in the tight corridor (narrow gap of bone) – this can result in damage to the protective covering of the nerve.
If the protective covering of the nerve becomes damaged, the signals which are being sent from the brain to the muscles in the face may not be transmitted properly, leading to weakened or paralyzed facial muscles – Bell’s palsy.
How is Bell’s palsy diagnosed?
Diagnosing by a process of elimination (diagnosis of exclusion)
The doctor will look for evidence of other conditions which may be causing the facial paralysis, such as a tumor, Lyme disease, or stroke. This will involve checking the patients head, neck and ears. He/she will also check the facial muscles carefully and determine whether any other nerves are affected apart from the facial nerve.
If there is a change in facial structure it could be evidence of a tumor. A characteristic rash may be evidence of tick bites in Lyme disease.
If all other causes can be excluded, the doctor will diagnose Bell’s palsy. If the doctor is still unsure, the patient may be referred to an ENT (ear, nose and throat) specialist – an otolaryngologist. The specialist will examine the patient and may also order the following tests:
- Electromyography (EMG) – electrodes are placed on the patient’s face. A machine measures the electrical activity of the nerves – and the electrical activity of a muscles in response to stimulation. This test can determine the extent of nerve damage, as well as its location.
- MRI, CT scans or X-rays – these are good at determining whether other underlying conditions are causing the symptoms, such as a bacterial infection, skull fracture, or a tumor.
What are the complications of Bell’s palsy?
It is important to stress that the vast majority of patients with Bell’s palsy make a full recovery. However, if damage to the facial nerve is severe some complications are possible, including:
- Misdirected re-growth of nerve fibers – nerve fibers re-grow in an irregular way. This can result in involuntary contractions of some muscles. A patient may involuntarily close one eye when trying to smile. The problem might be the other way round – when the person closes one eye, the side of the mouth lifts involuntarily.
- Ageusia – chronic (long-lasting) loss of taste.
- Gustatolacrimal reflex – also known as crocodile tear syndrome. While the patient is eating his/her eye will shed tears. It is estimated to occur in about 6% of patients during recovery, and eventually goes away. In some rare cases the problem can be longer lasting.
- Corneal ulceration – when eyelids cannot completely shut, the protective and lubricating tear film of the eye may become ineffective. This can result in corneal drying. The risk or corneal drying is even higher if Bell’s palsy has also caused a reduction in tear production. Corneal ulceration can result in infection of the cornea, which can lead to severe loss of vision.
How Can a Physical Therapist Help?
In the first couple of days to a week after symptoms start, your physical therapist will evaluate your condition, including:
- Review your medical history, and discuss any previous surgery or health conditions
- Review when your current symptoms started and what makes them worse or better
- Conduct a physical examination, focusing on identifying the patterns of weakness that are caused by Bell palsy:
- Facial movements of the eyebrow
- Eye closure
- Ability to use the cheek in smiling
- Ability to use the lips in a pucker
- Ability to suck the cheeks between the teeth
- Raising the upper lip
- Raising or lowering the lower lip
Your physical therapist will immediately:
- Educate you about how to protect your face and your eye
- Show you how to manage your daily life functions while you have facial paralysis
- Explain the expected path to recovery, so that you will know the signs and symptoms of recovery
- Evaluate your progress, and determine whether you need to be referred to a specialist if progress is not being made
The first priority is to protect your eye. The inability to completely and quickly close your eye makes the eye vulnerable to injury from dryness and debris. Debris can scratch the cornea—the transparent front part of the eye that covers the iris, pupil, and front chamber of the eye—and could permanently harm your vision. Your physical therapist will immediately show you how to protect your eye, such as:
- Using self-made and commercial patches
- Setting a regular schedule for refreshing eye fluids
- Carefully closing the eye with your fingers
If you have partial facial movement, your therapist will teach you a few general facial exercises to do at home. These exercises will help you learn to move the weak side of your face and help you use both sides of your face together. One of the exercises is a gentle blowing action through your lips.
During Recovery
Your physical therapist will help you regain the healthy pattern of movements that you need for facial expressions and function. Recovery can be challenging because:
- Normally, the ability to make facial expressions and many facial movements is “automatic”;—that is, you’re born with this ability and never had to think about it before
- Unlike other muscles in your body, the facial muscles do not have sensors that tell your brain all of the necessary “details” about how to move
Your physical therapist will be your coach throughout this challenging time, guiding you through special exercises that are designed to help you relearn facial movements based on your particular movement problems. Your exercises may change over the course of recovery:
“Initiation” exercises. In the early stages, when you might have difficulty producing any facial movement at all, your therapist will teach you exercises that cause (“initiate”) facial movement. Your therapist will show you how to position your face to make it easier to move (called “assisted range of motion”) or how to “trigger” the facial muscles to do what you want them to do.
“Facilitation” exercises. Once you’re able to initiate movement of the facial muscles, your therapist will design exercises to increase the activity of the muscles, strengthen the muscles, and improve your ability to use the muscles for longer periods of time (“facilitate” muscle activity).
Movement control exercises. Your therapist will design exercises to:
- Improve the coordination of your facial muscles
- Refine your facial movements for specific functions, such as speaking or closing your eye
- Refine movements for facial expressions, such as smiling
- Correct abnormal patterns of facial movement that can occur during recovery
To work on coordinating your facial muscles, you’ll need to have a sufficient level of activation of facial muscles first. Your therapist will determine when you’re ready.
Relaxation.During recovery, you might have facial spasms or twitches. Your physical therapist will design exercises to reduce this unwanted muscle activity. The therapist will teach you how to recognize when you are activating the facial muscle and when the muscle is at rest. By learning to contract the facial muscle forcefully and then stop, you will be able to relax your facial muscles at will and decrease twitches and spasms.
After Recovery
Some people might have greater difficulty moving their face after a period of improvement in facial movement, which can make them worry that the facial paralysis is returning. However, actual recurrence of facial paralysis of the Bell Palsy type is uncommon.
New difficulty in moving the face is more likely the result of increasing the strength of the facial muscles without improving the ability to coordinate and control the movement. To keep this from happening, your physical therapist will show you what facial movements you should avoid during recovery. For instance, the following might lead to abnormal patterns of facial muscle use:
- Trying to make the biggest facial movement or muscle contraction that you can, such as smiling as much as you can
- Chewing gum with great force
- Blowing up a balloon with all of your effort to work the facial muscles
Your therapist will coach you to use your face as naturally as possible, without trying to restrict facial expressions because they look “different.”
Reference:
Medical News Today http://www.medicalnewstoday.com/articles/158863.php
Move Forward http://www.moveforwardpt.com/symptomsconditionsdetail.aspx?cid=96135873-1b28-48bc-8be7-7d05c334daf1
[tagline_box link=”http://www.rehabexperts.com.ph/contact-us” linktarget=”” button=”Contact us now!” title=”Physical Therapy Home Service” description=”Are you a person suffering from some physical disabilities? Do you intend to find a solution to your physical disabilities? Are you already tired masking the pain and intend to find a solution to your physical disabilities? Do you intend to address the root-cause of pain and find a lasting remedy to your physical disabilities? Are you looking for a good quality physical therapy home service?”][/tagline_box]
The post What Is Bell’s Palsy? What Causes Bell’s Palsy? appeared first on Rehab Experts.
]]>The post Carpal Tunnel Syndrome appeared first on Rehab Experts.
]]>Carpal tunnel syndrome most commonly occurs in women, with those aged between 30 and 60 years having the highest rates of the condition. Initial treatment aims to reduce and manage symptoms without surgery but if this is unsuccessful, surgery may be recommended.
Signs and symptoms
The onset of CTS symptoms is usually gradual and can affect either one or both hands. The most common symptoms are numbness and tingling of the hand and fingers. Other symptoms may include:
- Burning, prickly, pin-like sensations in the hand and fingers
- Hand stiffness – particularly in the morning
- A feeling of swelling in the fingers – even though they may not be visibly swollen
- Wasting of the muscles in the hand can occur in long-term (chronic) cases
- Weakened grip
- Pain in the hand and fingers. The pain may: be intermittent or constant; worsen at night; worsen with increased use of the hand; radiate from the hand to the forearm or shoulder.
What causes carpal tunnel syndrome?
- In most cases it is not clear why it occurs. It is thought that some minor changes occur in the tendons and/or other structures going through the carpal tunnel. This may cause an increase in pressure within the tunnel. The increase in pressure is thought to compress and restrict the blood supply to the median nerve. As a result, the function of the median nerve is affected causing the symptoms. Carpal tunnel syndrome is more common in manual workers, especially with jobs using a lot of wrist movement such as scrubbing or wringing. So, overuse of the hand may be a factor in some cases to trigger the changes in the structures in the carpal tunnel, leading to this condition developing.
- Your genes may play a part. There seems to be some hereditary (genetic) factor. About 1 in 4 people with carpal tunnel syndrome has a close family member (father, mother, brother, sister) who also has or had the condition.
- Bone or arthritic conditions of the wrist such as rheumatoid arthritis or wrist fractures may lead to carpal tunnel syndrome.
- Various other conditions are associated with carpal tunnel syndrome. For example: pregnancy, obesity, an underactive thyroid, diabetes, the menopause, other rare diseases, and a side-effect of some drugs. Some of these conditions cause water retention (oedema) which may affect the wrist and cause carpal tunnel syndrome.
- Rare causes include cysts, growths, and swellings coming from the tendons or blood vessels passing through the carpal tunnel.
Doctor Examination
To determine whether you have carpal tunnel syndrome, your doctor will discuss your symptoms and medical history. He or she will also examine your hand and perform a number of physical tests, such as:
- Checking for weakness in the muscles around the base of your thumb
- Bending and holding your wrists in positions to test for numbness or tingling in your hands
- Pressing down on the median nerve in the wrist to see if it causes any numbness or tingling
- Tapping along the median nerve in the wrist to see whether tingling is produced in any of the fingers
- Testing the feeling in your fingers by lightly touching them when your eyes are closed
Do I need any tests?
Often the symptoms are so typical that no tests are needed to confirm the diagnosis.
If the diagnosis is not clear then a test to measure the speed of the nerve impulse through the carpal tunnel may be advised (nerve conduction test). A slow speed of impulse down the median nerve will usually confirm the diagnosis.
How Can a Physical Therapist Help?
After the evaluation, your physical therapist will prescribe your treatment plan based on your specific case.
Conservative Care
If your evaluation confirms early-stage CTS, conservative care will be recommended as a first step. Physical therapy treatment can be effective in reducing your symptoms and getting you back to performing normal activities. During your first visit with the physical therapist, be prepared to describe your symptoms in as much detail as possible, and say what makes your symptoms worse.
Depending upon the causes of your CTS, your therapy program may include:
- Education regarding:
- changing wrist positions (ie, avoiding prolonged bent wrist positions)
- proper neck and upper back posture (ie, avoiding forward head or slouching)
- safe use of sharp utensils, tools, or other implements, if sensory changes are identified
- “stretch breaks” during your work or daily routine
- Exercises to increase the strength of the muscles in your hand, fingers, and forearm—and in some cases, the trunk and postural back muscles
- Stretching exercises to improve the flexibility of the wrist, hand, and fingers
- Use of heat/cold treatments to relieve pain
- Use of a night splint to reduce discomfort
- A worksite visit to assess your work area. For example, if you sit at a desk and work on a computer, it’s important for the keyboard to be in proper alignment to help avoid working in a bent wrist position.
- Increasing the size of tool and utensil handles by adding extra material for a more comfortable grip
- Anti-vibration gloves or anti-vibration wraps around tool handles, if vibration is a factor at your workplace
Your physical therapist will also consider your home and leisure activities, with recommendations such as wearing gloves to keep the wrist/hands warm and limiting sports that aggravate the condition, such as racquet sports, until symptoms resolve.
The goals of physical therapy are to reduce your symptoms without the need for surgery, to enable you to be as active and functional as possible, and to help you resume your normal work, home, and leisure activities.
Physical Therapy Following Surgery
If the evaluation reveals that your CTS is more severe, or if your symptoms persist, your physical therapist may refer you to a physician for a surgical consultation. If necessary, surgery will be performed to release the band of tissue that is causing pressure on the median nerve. Physical therapy treatment is important after surgery to help restore strength to the wrist and to learn to modify habits that may have led to symptoms in the first place. Your physical therapy treatment may include:
- Exercises to improve the strength of the wrist/hand muscles and improve function
- Stretching to improve mobility of the wrist/fingers and improve function
- Scar management to keep the skin supple and flexible
- Education regarding appropriate posture and wrist position to avoid carpal tunnel compression in home/leisure activities
- A worksite visit or simulation to optimize postures and positions
Reference:
Southern Cross Healthcare Group https://www.southerncross.co.nz/AboutTheGroup/HealthResources/MedicalLibrary/tabid/178/vw/1/ItemID/203/Carpal-tunnel-syndrome-CTS.aspx
Ortho Info http://orthoinfo.aaos.org/topic.cfm?topic=a00005
Patient.Co.UK http://www.patient.co.uk/health/carpal-tunnel-syndrome
Move Forward http://www.moveforwardpt.com/symptomsconditionsdetail.aspx?cid=9f3cdf74-3f6f-40ca-b641-d559302a08fc
The post Carpal Tunnel Syndrome appeared first on Rehab Experts.
]]>The post Postural Problems appeared first on Rehab Experts.
]]>Postural problems can affect individuals at any age, for example a baby may be born with a genetic condition or an abnormality in the spine such as congenital scoliosis (when the spine bends to one side) that causes postural problems.
Teenagers may develop postural problems as they become more aware and conscious of themselves and develop tendencies to hunch or slouch.
Symptoms of scoliosis often start showing in children and teenagers and can also cause them to hunch or slouch and not be able to stand straight.
Adults may develop postural problems as a result of incorrect posture at work while at a desk or computer for prolonged periods of time, while arthritis and osteoporosis suffers can also experience postural problems as joints become inflamed and swollen and bones become brittle.
Commonly postural problems develop when muscles become tight and stressed or weak and lax and the body is not correctly supported. Poor posture can also cause stress and weakness of muscles creating a cycle of problems.
What Causes Posture Problems?
Poor posture may be caused by many factors, including previous injuries, disease, poor muscle tone, and emotional stress. A sedentary lifestyle can reduce muscle tone and strength and lead to bad posture. Sore, aching feet have a negative effect on posture, too. Foot pain may mean simply that you’re choosing the wrong shoes. Or you may need special supports—orthotic devices—in your shoes. One very important factor is habit. Contrary to what some people believe, straightening up now and then isn’t enough: you need to be aware of—and to practice—other strategies to improve standing and sitting. In addition, fatigue can result in bad posture.
What If You Do Nothing?
In itself, poor posture isn’t a health problem. But it won’t improve without some effort on your part, and in the meantime it can have an adverse impact on your musculoskeletal system. If you don’t take steps to improve your posture, you may eventually limit your lung expansion—which means less energy available to your body and brain—and develop chronic muscle aches, including headaches and back pains.
Diagnosis of Postural Problems
Diagnosis of postural problems often begins when an individual, or a friend or family member recognises that a person is not standing straight or sitting upright and the individual may feel pain and discomfort.
Individuals should seek advice from their doctor about correct posture and treatment which may include being referred to a physical therapist for exercises and advice to alleviate postural problems.
The doctor may ask the individual about their profession and day to day environment and may ask them to sit and stand to assess their posture. If needed the doctor may recommend an X-ray, MRI or CT scan to further diagnose postural problems.
Conditions such as scoliosis are diagnosed usually through a physical exam of the spine and for children examining the shoulders and hips as well. This is then followed by an x-ray or MRI scan.
5 Most Common Posture Problems (and how to fix them)
Posture Problem #1: Over-Pronated Feet
Identification – As shown in the photo above, put both hands 1 inch away from each side of your foot. Straighten your ankle so that the space between each hand and your ankle is equidistant. Now naturally let your ankle and feet rest. If your foot and ankle caved inward, you have over-pronated feet.
Causes – Obesity, pregnancy, improper footwear, or repetitive pounding on a hard surface can weaken the arch leading to over-pronation and oftentimes flat feet.
Problem – Over-pronation adds stress to the foot, tightens calf muscles, and can internally rotate the knees. Over-pronation often leads to Plantar Fasciitis, Heel Spurs, Metatarsalgia, Post-tib Tendonitis and/or Bunions.
Solution – If the arch has already fallen, orthotics are the best bet. If the arch is in the process of falling, or is weak, barefoot running/walking may help strengthen the arches, but be sure to check with your doctor (orthotics may be the best bet in this case as well).
Posture Problem #2: Forward Hip Tilt
Identification – Identifying a forward tilt can be tricky, but one method is to purposely tilt your pelvis forward as far as you can, then backward as far as you can. You may realize your natural hip tilt is not far away from the exaggerated forward tilt.
Cause – Sitting too much and not stretching, which shortens the hip flexors
Problem – Forward hip tilt (aka anterior pelvic tilt) is associated with tight hip flexors, which are a group of muscles on the front of your hips that pull the knee upward. As you walk, tight hip flexors prevent the glutes (butt muscles) from firing/activating, which forces the hamstring muscles to become overworked and excessively tight. If you have tight hamstrings, the root cause may be tight hip flexors and an anterior pelvic tilt.
Solution – Stretch your hip flexors with static lunges, such as the Crescent Lunge, activate your glutes with exercises like glute bridges, and foam roll and stretch your hamstrings.
Posture Problem #3: Hunchback
Identification – Have someone take a photo of you standing sideways. If you notice that your upper back is excessively curved (greater than 40-45 degrees) as in the photo to the right, you have hunchback posture.
Cause – Sitting with bad posture, especially at an office doing computer work
Problem – Sitting hunched over a computer screen forces chest muscles to tighten, which can cause excessive curvature (kyphosis) of the upper back (thoracic spine). Postural muscles in the upper back weaken and loosen.
Solution – Relieve chest tightness with self myofascial release (use a massage ball) and stretching, while strengthening the upper back postural muscles.
Posture Problem #4: Rounded Shoulders
Identification – The “Pencil Test” involves holding a pencil (or pen) in each hand. As shown in the photo above, if the pencils are pointing straight forward with your arms comfortably at your sides, that indicates correct posture. If on the other hand the pencils are facing each other, or are rotated at an angle, then you have internally rotated shoulders.
Cause – Sitting with bad posture, especially in an office while typing, or using an imbalanced exercise routine with excessive chest pressing.
Problem – Sitting hunched over a computer screen forces chest muscles to tighten, which can internally rotate the shoulders forward. Postural muscles in the upper back weaken and loosen.
Solution – The solution is very similar to correcting hunchback posture – relieve chest tightness with self myofascial release (use a massage ball) and stretching, while strengthening the upper back postural muscles.
Posture Problem #5: Forward Head
Identification – Have someone take a photo of you standing sideways. As shown in the photo to your right, find the AC joint (bony protrusion on the side of your shoulder) and check if your ear lobe is on top of the AC joint. If your ear lobe extends in front of your AC joint, you have a forward head posture.
Cause – Sitting in an office chair hunched over while staring at a computer
Problem – Muscles in the back of the neck become tight, along with the upper trapezius and levator scapulae (upper back muscles).
Solution – First, practice proper head posture by sliding your head backward while keeping your line of sight ahead. Be sure not to tilt your head upwards as you slide your head back. Second, get a massage, or use a massage ball against your upper back, which can be very helpful to help relieve tension around your neck.
PHYSICAL THERAPY AND POSTURE
In the practice of physical therapy posture is a concept frequently used in examining people and determining if treatment, particularly for back and neck problems, has made any changes in a person. Posture is defined as “the position or bearing of the body” and refers to the overall alignment of the various body parts to each other when the person is standing in a relaxed stance.
At Rehab Experts your therapist will take a detailed history and evaluation. Your therapist will assess the strength, sensation, and circulation in the affected areas. They will gauge your balance, gait, posture, and range of motion.
Exercises for stability, balance, posture, flexibility, coordination, range of motion, and strength will be assigned to ensure that you are returned to a normal lifestyle as soon as possible.
Reference:
Therapy Web http://www.therapyweb.co.uk/problems/postural-problems#Causes
Health Communities http://www.healthcommunities.com/back-pain/posture-problems.shtml
Built Lean http://www.builtlean.com/2011/11/28/posture-problems/
The Posture Page http://www.posturepage.com/pt/
The post Postural Problems appeared first on Rehab Experts.
]]>